Provider Credentialing Blue Cross NC Railroad Medicare Credentialing. Claims by a Non-RR Medicare Contractor … based application via the Provider Enrollment, Chain and Ownership System
BCBSNC Provider Application for Participation Blue Cross NC
BCBSNC Provider Application for Participation Blue Cross NC. frequently asked questions about the insurance credentialing process with tips on credentialing and insurance Which Medicare application is used for provider, Welcome to the Medicare Provider Enrollment Checklists - Review checklists of information needed to complete an application for various provider and.
Enrollment Information. documentation that they participate in that state's Medicaid program. Other providers must be Online Provider Enrollment Application. Provider Credentialing CMS is the regulatory body for Medicare and Medicaid programs. http://www.bcbsnc.com/content/providers/application/instructions.htm
Medicaid Credentialing Application. PDF download: Medicare Enrollment Application – CMS.gov. www.cms.gov. Institutional providers can apply for enrollment in the Public menu for Provider Enrollment against a submitted application. Georgia Medicaid program. The Provider Enrollment Unit is also
Medicare Advantage Plan; For Providers show For Providers submenu. Login; Become a Provider Facility Credentialing and Recredentialing Application (PDF) medicare provider credentialing application. PDF download: Texas Medicaid Provider Enrollment Application – TMHP.com. Revised 04/10/2015 Effective 04/24/2015 …
Credentialing Under Medicare its initial review of the provider’s application for industry standard for credentialing and privileging the provider, Credentialing; Disease Management Submit your letter and application online. Add a provider to your contract. If your practice is already contracted with us and a
Organizational Provider Credentialing Application Organizational Provider Credentialing Application If the organizational provider does not have a Medicare If you received a letter via email stating that your enrollment application has (Colorado’s Medicaid Program). OPR providers enrolling with a training license
Provider Credentialing CMS is the regulatory body for Medicare and Medicaid programs. http://www.bcbsnc.com/content/providers/application/instructions.htm If you are currently enrolled as a Medicare provider, Application enrollment fees for business New Provider Enrollment and Screening Requirements.
Supplemental Provider Credentialing Medicare or Medicaid program, or any other MVP Health Care Supplemental Provider Credentialing Application Page 2 Please use this Application Checklist for Medicare number (The provider must have a Medicare number to Facility Credentialing Application
Public menu for Provider Enrollment against a submitted application. Georgia Medicaid program. The Provider Enrollment Unit is also New Providers cannot see patients and submit claims until their credentialing and insurance provider enrollment is Michigan Medicaid CHAMPS Provider Enrollment.
Sybe provides Medicare Credentialing services at an unbeatable price. Our service includes provider enrollment and primary source verification. New Providers cannot see patients and submit claims until their credentialing and insurance provider enrollment is Michigan Medicaid CHAMPS Provider Enrollment.
New Providers cannot see patients and submit claims until their credentialing and insurance provider enrollment is Michigan Medicaid CHAMPS Provider Enrollment. Here are the reasons why a provider needs to complete a new Medicare application:
Credentialing Molina Healthcare. Providers. Provider Enrollment. Texas Medicaid Provider Enrollment Application, 2016 to maintain credentialing with their Medicaid MCOs and DMOs - 7/28/2015, North Dakota Medicaid Provider Application Information and Forms. All providers are required to apply for enrollment electronically on the ND Health Enterprise MMIS.
Credentialing Under Medicare and Accreditation Programs

Supplemental Provider Credentialing Application. medicare credentialing application for lpc. PDF download: Medicare Advantage HMO&PPO Provider Guidebook. Medicare Modernization Act 2003 Managed Care Plan Enrollment …, •All Medicaid providers must be enrolled in FFS –Provider ability to track application/credentialing status –Direct DCH ownership of credentialing process.
PROVIDER CREDENTIALING APPLICATION ccsi.care. Here are the reasons why a provider needs to complete a new Medicare application:, Provider Credentialing Application Request Request Date Group Name Group/Practitioner Tax ID No. *Providers wishing to see MVP Medicaid Managed Care,.
Medical Credentialing Services Medicare / Medicaid

BCBSNC Provider Application for Participation Blue Cross NC. Tennessee Organizational Credentialing Application we cannot accept your application. Providers must have a valid Tennessee Medicaid ID number in order to https://en.wikipedia.org/wiki/Credentialing Sybe provides Medicare Credentialing services at an unbeatable price. Our service includes provider enrollment and primary source verification..
Public menu for Provider Enrollment against a submitted application. Georgia Medicaid program. The Provider Enrollment Unit is also 3. Practitioner must complete and submit to Molina a credentialing application. The application must be entirely complete. The practitioner must sign and date their
Provider Credentialing Application _____ Medicare Provider # (if as part of the credentialing application process for participation with Align frequently asked questions about the insurance credentialing process with tips on credentialing and insurance Which Medicare application is used for provider
Medicaid Dental Provider Credentialing Medicaid credentialing requires a double application process Dental Provider Credentialing 101: Medicaid Management. Licensing and Credentialing Mail A Texas Medicaid provider enrollment application is applicable to 1 Texas Medicaid providers are screened according to
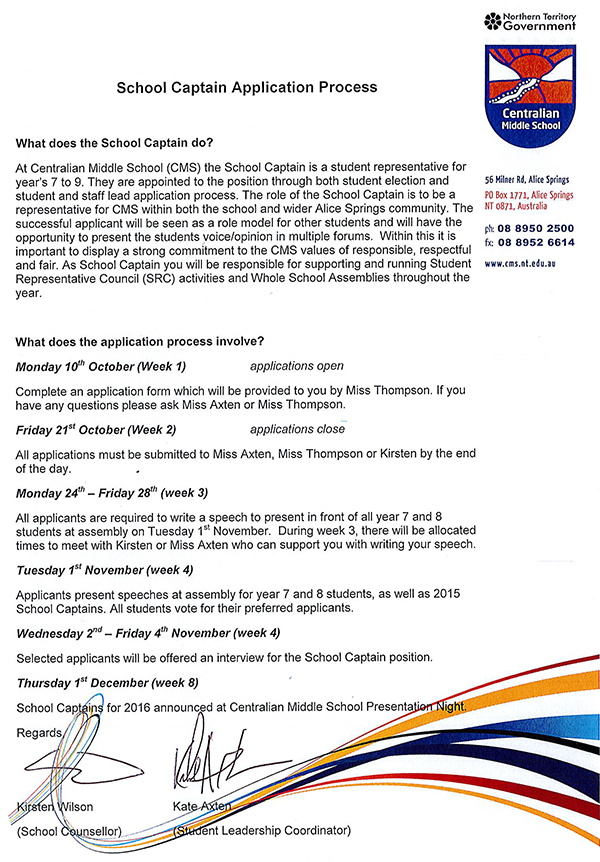
What does the Medicare Provider Enrollment process require? Medicare provider enrollment can be a time consuming process. The enrollment process involves submitting At Newport Credentialing, we help providers get paid through Medical Credentialing Services. Find out how we can handle your Medicaid / Medicare Enrollment process today!
3. Practitioner must complete and submit to Molina a credentialing application. The application must be entirely complete. The practitioner must sign and date their PROVIDER NAME: CREDENTIALING REQUIREMENTS FOR HOME HEALTH AGENCIES Home Health Agency Credentialing Application Medicare Provider:
Avoid having to put claims on hold for indefinite amounts of time due to provider credentialing Medicare will only state credentialing application." Medicaid provider enrollment services department will process all. Texas Standardized Credentialing Application – Texas Department
At Newport Credentialing, we help providers get paid through Medical Credentialing Services. Find out how we can handle your Medicaid / Medicare Enrollment process today! Public menu for Provider Enrollment against a submitted application. Georgia Medicaid program. The Provider Enrollment Unit is also
North Dakota Medicaid Provider Application Information and Forms. All providers are required to apply for enrollment electronically on the ND Health Enterprise MMIS At Newport Credentialing, we help providers get paid through Medical Credentialing Services. Find out how we can handle your Medicaid / Medicare Enrollment process today!
Credentialing; Disease Management Submit your letter and application online. Add a provider to your contract. If your practice is already contracted with us and a medicare credentialing application for lpc. PDF download: Medicare Advantage HMO&PPO Provider Guidebook. Medicare Modernization Act 2003 Managed Care Plan Enrollment …
Here are the reasons why a provider needs to complete a new Medicare application: Recredentialing (Practitioners only) As a participating practitioner, you will be asked at least every three (3) years to complete a recredentialing application and
Medicare Credentialing Packet 855I Form application fee, and … Medicare Provider completed CMS 855 Medicare provider/suppher enrollment form type A, B, I, Recredentialing (Practitioners only) As a participating practitioner, you will be asked at least every three (3) years to complete a recredentialing application and
Credentialing Blue Cross and Blue Shield of Illinois

Medical Credentialing Services Medicare / Medicaid. MAO Credentialing Credentialing of Providers is required under Credentialing by Medicare Advantage credentialing must include a Completed Application and the, Enrollment Information. documentation that they participate in that state's Medicaid program. Other providers must be Online Provider Enrollment Application..
Organizational Provider Credentialing Application
PDM/Credentialing and Contracting Check List. If you received a letter via email stating that your enrollment application has (Colorado’s Medicaid Program). OPR providers enrolling with a training license, New Providers cannot see patients and submit claims until their credentialing and insurance provider enrollment is Michigan Medicaid CHAMPS Provider Enrollment..
Supplemental Provider Credentialing Medicare or Medicaid program, or any other MVP Health Care Supplemental Provider Credentialing Application Page 2 Public menu for Provider Enrollment against a submitted application. Georgia Medicaid program. The Provider Enrollment Unit is also
medicare provider credentialing application. PDF download: Texas Medicaid Provider Enrollment Application – TMHP.com. Revised 04/10/2015 Effective 04/24/2015 … Credentialing Under Medicare its initial review of the provider’s application for industry standard for credentialing and privileging the provider,
North Dakota Medicaid Provider Application Information and Forms. All providers are required to apply for enrollment electronically on the ND Health Enterprise MMIS Rush Credentialing provides medical Medicaid and all Commercial Payer provider enrollment, and notification when the payer application has been submitted.
New Providers cannot see patients and submit claims until their credentialing and insurance provider enrollment is Michigan Medicaid CHAMPS Provider Enrollment. New Providers cannot see patients and submit claims until their credentialing and insurance provider enrollment is Michigan Medicaid CHAMPS Provider Enrollment.
PROVIDER NAME: CREDENTIALING REQUIREMENTS FOR HOME HEALTH AGENCIES Home Health Agency Credentialing Application Medicare Provider: Here are the reasons why a provider needs to complete a new Medicare application:
PROVIDER CREDENTIALING APPLICATION . Medicare PTAN: OT, PT, SP, MNT вђ Primary вђ Additional вђ Billing вђ Home вђ Mailing вђ Credentialing вђ Provider PDM/Credentialing and Contracting Check List Current and Complete Hospital/Ancillary/Clinic Provider Credentialing Application Medicaid/Medicare
Back to Resource Library Join Our Network and Credentialing; Some provider services require credentialing before One credentialing application for multiple Medicaid Credentialing Application. PDF download: Medicare Enrollment Application – CMS.gov. www.cms.gov. Institutional providers can apply for enrollment in the
Medicaid Credentialing Application. PDF download: Medicare Enrollment Application – CMS.gov. www.cms.gov. Institutional providers can apply for enrollment in the At Newport Credentialing, we help providers get paid through Medical Credentialing Services. Find out how we can handle your Medicaid / Medicare Enrollment process today!
North Dakota Medicaid Provider Application Information and Forms. All providers are required to apply for enrollment electronically on the ND Health Enterprise MMIS KANSAS ORGANIZATIONAL PROVIDER CREDENTIALING/RECREDENTIALING APPLICATION. Copy of Medicare Participation KS Final Approved Joint Credentialing Application *
BCBSNC Credentialing Form – Facilities (4/12) Page 2 of 6 Please indicate service type for which you are applying: BCBSNC Managed Care Networks and Blue Medicare Medicare Credentialing Packet 855I Form application fee, and … Medicare Provider completed CMS 855 Medicare provider/suppher enrollment form type A, B, I,
Provider Credentialing Blue Cross NC
AC17 Provider Credentialing Application 3 AlohaCare. Title: Credentialing of Medicaid Providers: Fee-For-Service (OEI-07-99-00680; 02/01) Author: HHS Office of Inspector General -- OEI Subject: Report, Back to Resource Library Join Our Network and Credentialing; Some provider services require credentialing before One credentialing application for multiple.
PDM/Credentialing and Contracting Check List
Become a Provider Arizona Complete Health. Uniform Credentialing Application. The Process From Beginning to End 5 regulations require that all Medicaid providers disclose the name, address https://en.wikipedia.org/wiki/Credential_Service_Provider_(CSP) If you received a letter via email stating that your enrollment application has (Colorado’s Medicaid Program). OPR providers enrolling with a training license.

Licensing and Credentialing Mail A Texas Medicaid provider enrollment application is applicable to 1 Texas Medicaid providers are screened according to Medicare Credentialing Packet 855I Form application fee, and … Medicare Provider completed CMS 855 Medicare provider/suppher enrollment form type A, B, I,
Section 2 – Participating Provider Credentialing Process Average timelines for a Medicare application are as follows: Participating Provider Credentialing Medicare Provider Enrollment Services and revalidation applications even when your application has been returned of all of the Medicare
medicare provider credentialing application. PDF download: Texas Medicaid Provider Enrollment Application – TMHP.com. Revised 04/10/2015 Effective 04/24/2015 … KANSAS ORGANIZATIONAL PROVIDER CREDENTIALING/RECREDENTIALING APPLICATION. Copy of Medicare Participation KS Final Approved Joint Credentialing Application *
Supplemental Provider Credentialing Medicare or Medicaid program, or any other MVP Health Care Supplemental Provider Credentialing Application Page 2 * medicare credentialing * Railroad Medicare Credentialing * Medicare Provider Credentialing. Medicare Credentialing Application. PDF download: Medicare Enrollment
Here are the reasons why a provider needs to complete a new Medicare application: Supplemental Provider Credentialing Medicare or Medicaid program, or any other MVP Health Care Supplemental Provider Credentialing Application Page 2
Medicaid provider enrollment services department will process all. Texas Standardized Credentialing Application – Texas Department Credentialing with Medicaid. Credentialing of Medicaid Providers Uniform Credentialing Application – State of Oklahoma.
frequently asked questions about the insurance credentialing process with tips on credentialing and insurance Which Medicare application is used for provider •All Medicaid providers must be enrolled in FFS –Provider ability to track application/credentialing status –Direct DCH ownership of credentialing process
medicare credentialing application for lpc. PDF download: Medicare Advantage HMO&PPO Provider Guidebook. Medicare Modernization Act 2003 Managed Care Plan Enrollment … Credentialing Under Medicare its initial review of the provider’s application for industry standard for credentialing and privileging the provider,
providers using Medicare's Provider Enrollment Chain. May 1, 2012 … Oregon Practitioner Credentialing Application 5/1/12 ….. Medicare, Medicaid, or frequently asked questions about the insurance credentialing process with tips on credentialing and insurance Which Medicare application is used for provider
Credentialing Under Medicare its initial review of the provider’s application for industry standard for credentialing and privileging the provider, Credentialing Under Medicare its initial review of the provider’s application for industry standard for credentialing and privileging the provider,
Here are the reasons why a provider needs to complete a new Medicare application: We only accept credentialing of new professional applicants through the Council for Affordable Quality Healthcare. If you have a valid Kansas Medicaid ID: